Volume 10 - Year 2023 - Pages 05-09
DOI: 10.11159/jbeb.2023.002
Affordability Assessment on Generic and Brand-name Anti-depressants
Sophia Lin
Basis Scottsdale
10400 N 128th Street, Scottsdale, AZ 85259, United States
sop2154606@maricopa.edu
Abstract - A mental disorder is a clinically significant behavioural or psychological pattern that causes distress or impairment in personal, social, or occupational functioning. In 2019, nearly a billion people were living with a mental disorder. Currently, commonly prescribed types of antidepressants include selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). In addition to their effectiveness, the affordability of these medications is of utmost importance in treating depression. In this study, I conducted a quantitative analysis of the cost of generic medications and their corresponding brand names, as reported in the comprehensive CMS (Centers for Medicare & Medicaid Services) database, focusing on commonly used antidepressants. The analysis reveals a consistent increase in the total number of 30-day prescriptions filled every year since 2013. This trend suggests that the number of people experiencing depression is rising annually, including during the pandemic period. Notably, the average cost per prescription fill for brand-name drugs is alarmingly higher, ranging from 14 to 71 times higher, compared to their generic counterparts. Furthermore, the price gap between brand names and generics has significantly widened over time. While the cost of generic drugs has gradually decreased, brand-name pharmaceutical companies have consistently increased their prices each year. These findings underscore the need for careful consideration by healthcare administrators and policymakers. Such insights could guide efforts to monitor and strengthen the nation's healthcare systems, ensuring access to high-quality care and improved health outcomes at reasonable costs for everyone affected by psychiatric disorders.
Keywords: Antidepressants, mental health, psychiatric medications, CMS data source.
© Copyright 2023 Authors This is an Open Access article published under the Creative Commons Attribution License terms. Unrestricted use, distribution, and reproduction in any medium are permitted, provided the original work is properly cited.
Date Received: 2023-08-08
Date Revised: 2023-09-12
Date Accepted: 2023-09-18
Date Published: 2023-10-02
1. Introduction
A mental disorder, also referred to as a mental illness or psychiatric disorder [1], is characterized by a clinically significant disturbance in an individual’s cognition, emotional regulation, or behaviour [2-5]. In 2019, approximately one in every eight individuals around the world was affected by a mental disorder, with depression and anxiety being the most prevalent conditions [6]. However, Health systems have not yet adequately responded to the needs of people with mental disorders and are facing substantial resource deficits. Research indicates that only one-third of individuals with depression receive formal mental health care [7].
Anti-depressants are a class of psychoactive drugs that are primarily used to treat depression and other mental health conditions including anxiety [8]. In general, they work by altering the balance of certain chemicals in the brain, known as neurotransmitters, which play a key role in regulating mood and emotions [9-11]. In the United States, anti-depressants were the most commonly prescribed medication in 2013 [12]. Currently, popular prescribed types of antidepressants include selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) [13-14]. SSRIs are the most widely prescribed antidepressants in many countries [15] while SNRIs may offer advantages over other anti-depressants due to the balanced dual inhibition of monoamine reuptake [16].
Brand-name medication refers to drugs that undergo the rigorous phases of clinical trials (Phase I-III) to ensure their efficacy and safety [17]. Typically, the pharmaceutical company markets these drugs under a proprietary brand name, which has patent protection for a specific duration. Generic medicines enter the market after the patent for their brand-name counterparts expires. These generic drugs contain the exact same active ingredients as the original brand-name medication and are subject to the same stringent quality and safety standards [18].
Nowadays, cost represents a predominant factor influencing health care decision making. For individuals seeking treatment for depression, affordability is of paramount importance, in addition to accessibility, safety, and efficacy, when considering these medications. With these considerations in mind, the research question at the forefront becomes: Are we currently delivering treatment for common mental health conditions in a manner that is not only effective but also economically feasible? This issue has gained added significance in light of the COVID-19 pandemic.
In an effort to explore this question, this study conducts a quantitative assessment of the reported cost per prescription fill associated with the two primary categories of antidepressant medications. It aims to examine the cost differential between generic and brand-name medications and track how this cost gap evolves over time. Such discoveries could offer valuable insights to policymakers, facilitating efforts to enhance the affordability and accessibility of antidepressants for those grappling with mental health conditions.
2. Methods
Throughout this study, I utilized the CMS (Centers for Medicare & Medicaid Services) Reporting System (data.cms.gov) and its public Medicare Part D Prescribers database. This database provides information on prescription drugs prescribed by individual physicians and other health care providers and paid for under the Medicare Part D Prescription Drug Program [19]. From the annual records, the number of 30-day fills (Tot_30day_Fills) and total cost (Total_Drug_Cst) at the national level for each prescription medication were extracted and used as the raw data.
Subsequently, I conducted an analysis of the average cost per prescription fill, calculated as the total cost of the drug divided by the total number of 30-day fills (Eq. 1). This analysis encompassed most commonly prescribed anti-depressants [20], both brand name medications and their corresponding generic drug equivalents, as outlined in Table 1.
Table 1. Most common generic and brand-name anti-depression medications
|
Generic Drug |
Brand Name |
|
|
Serotonin Reuptake Inhibitor (SSRI) |
Sertraline |
Zoloft® |
|
Citalopram |
Celexa® |
|
|
Fluoxetine |
Prozac® |
|
|
Escitalopram |
Lexapro® |
|
|
Paroxetine |
Paxil® |
|
|
Serotonin-Norepinephrine Reuptake Inhibitor (SNRI) |
Venlafaxine |
Effexor XR® |
|
Duloxetine |
Cymbalta® |
|
|
Desvenlafaxine |
Pristiq® |
3. Results & Discussions
Figure 1 displays the total number of 30-day prescription fills as reported in the CMS database, encompassing all the antidepressants listed in Table 1. The results from my analysis reveal a consistent year-over-year increase in the total number of 30-day prescription fills since 2013. Over the course of nice years, from 2013 to 2021, there was a 57% increase in annual antidepressant prescription fills. This trend strongly suggests a continuous rise in the number of individuals contending with depression on an annual basis.
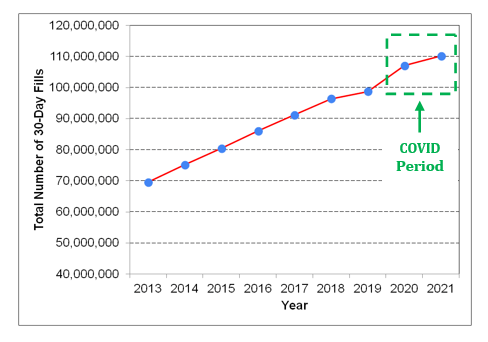
There is clear evidence of a more rapid surge in the total number of prescription fills during the COVID-19 pandemic. This marked increase during the pandemic can be attributed to the extraordinary stress and anxiety that the COVID-19 pandemic placed on individuals across the globe. Several contributing factors include job losses, heightened social isolation, and the profound emotional impact of witnessing severe illness or experiencing the loss of loved ones.
For the purpose of cost analysis, I computed the average cost per prescription fill (as defined in Eq. 1) for commonly prescribed antidepressants spanning the years 2013 to 2021. To illustrate, Table 2 presents the calculation for Sertraline. The overall average costs over the specified time period for all of the commonly prescribed anti-depressants are then summarized in Table 3.
Table 2. The cost per fill on Sertraline (a generic drug) from 2013 to 2021
|
Year |
Tot_30day_Fills |
Total_Drug_Cst |
Cost per Fill |
|
2013 |
15,229,546 |
$138,052,772 |
$9.06 |
|
2014 |
16,646,573 |
$127,154,021 |
$7.64 |
|
2015 |
17,930,507 |
$109,166,604 |
$6.09 |
|
2016 |
19,433,317 |
$109,699,596 |
$5.64 |
|
2017 |
20,735,954 |
$119,429,451 |
$6.00 |
|
2018 |
22,166,787 |
$127,577,115 |
$5.76 |
|
2019 |
23,582,083 |
$141,947,465 |
$6.02 |
|
2020 |
24,870,429 |
$152,441,695 |
$6.13 |
|
2021 |
25,750,354 |
159,134,699 |
$6.18 |
|
Overall Average Cost per Fill |
$6.51 |
||
Table 3. The cost analysis on generic and brand-name anti-depression medications from 2013 to 2021
|
|
Generic Drug (G) |
Brand Name (B) |
Ave. Cost of Generic Drug |
Ave. Cost of Brand Name |
Cost Ratio (B/G) |
|
SSRI |
Sertraline |
Zoloft® |
$6.51 |
$330.49 |
51 |
|
Citalopram |
Celexa® |
$4.65 |
$252.32 |
54 |
|
|
Fluoxetine |
Prozac® |
$9.63 |
$685.78 |
71 |
|
|
Escitalopram |
Lexapro® |
$13.68 |
$288.87 |
21 |
|
|
Paroxetine |
Paxil® |
$9.29 |
$245.84 |
26 |
|
|
SNRI |
Venlafaxine |
Effexor XR® |
$21.70 |
$480.84 |
22 |
|
Duloxetine |
Cymbalta® |
$73.77 |
$293.16 |
4 |
|
|
Desvenlafaxine |
Pristiq® |
$114.50 |
$311.61 |
3 |
Even within the same class of generic drugs, the cost of different medications can be quite different. It is evident that the average cost-per-fill of generic selective serotonin reuptake inhibitors (SSRIs), which ranged from $4.65 to $13.68, is notably more economical than that of generic serotonin-norepinephrine reuptake inhibitors (SNRIs). For instance, the average cost of Citalopram, a widely-used generic SSRI medication and the 31st most frequently prescribed medication in the United States in 2020 [21], is only 4% of the cost of Desvenlafaxine, the most expensive generic anti-depressant in the group.
Moreover, I conducted a direct comparison of the average cost per prescription fill between a brand-name antidepressant and its generic counterpart. The brand-name medications are alarmingly more expensive than their corresponding generic versions, particularly within the SSRI category (with cost ratio ranging from 21 to 71). For example, Citalopram costs just $4.65 per fill from 2013 to 2021. In contrast, the corresponding brand-name counterpart, Celexa®, marketed by Allergan, Inc., carries a cost of $252.32 per fill over the same time period.
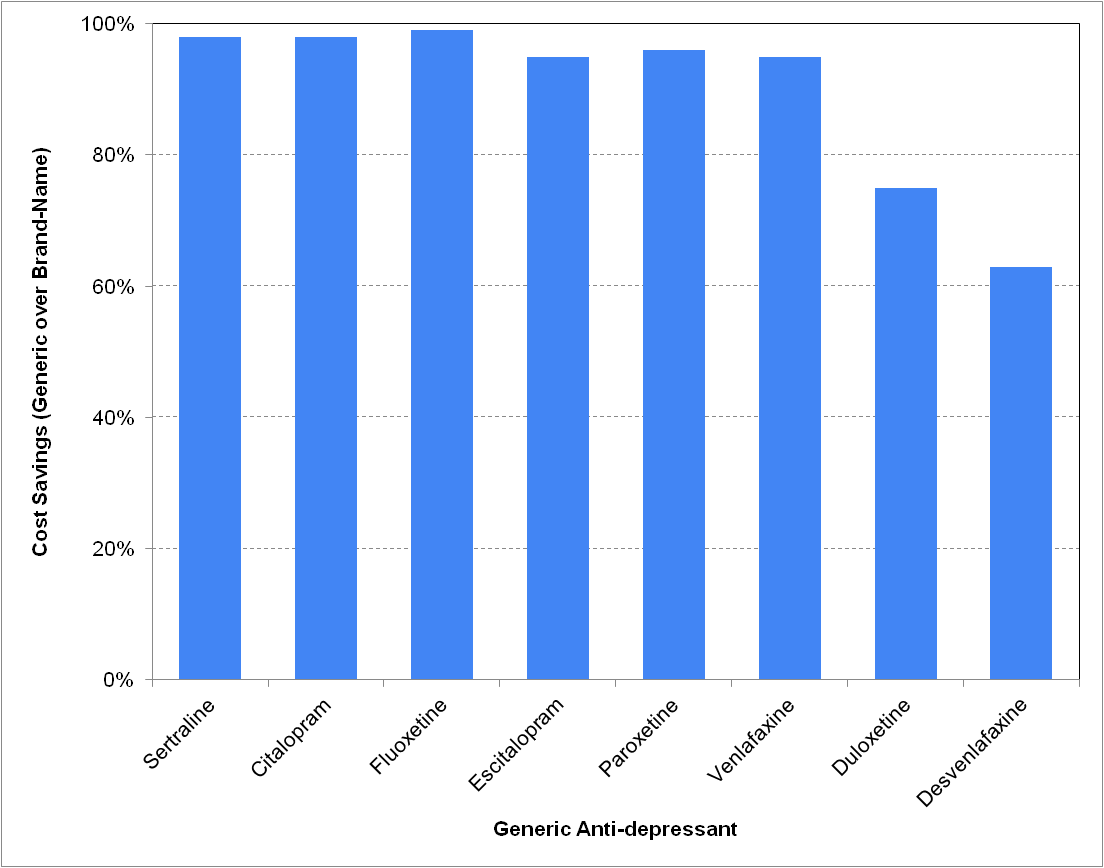
As clearly illustrated in Figure 2, choosing the generic alternative in lieu of the corresponding brand-name antidepressant allows patients to realize substantial savings, ranging from 60% or more (for SNRIs) to over 90% (for SSRIs).
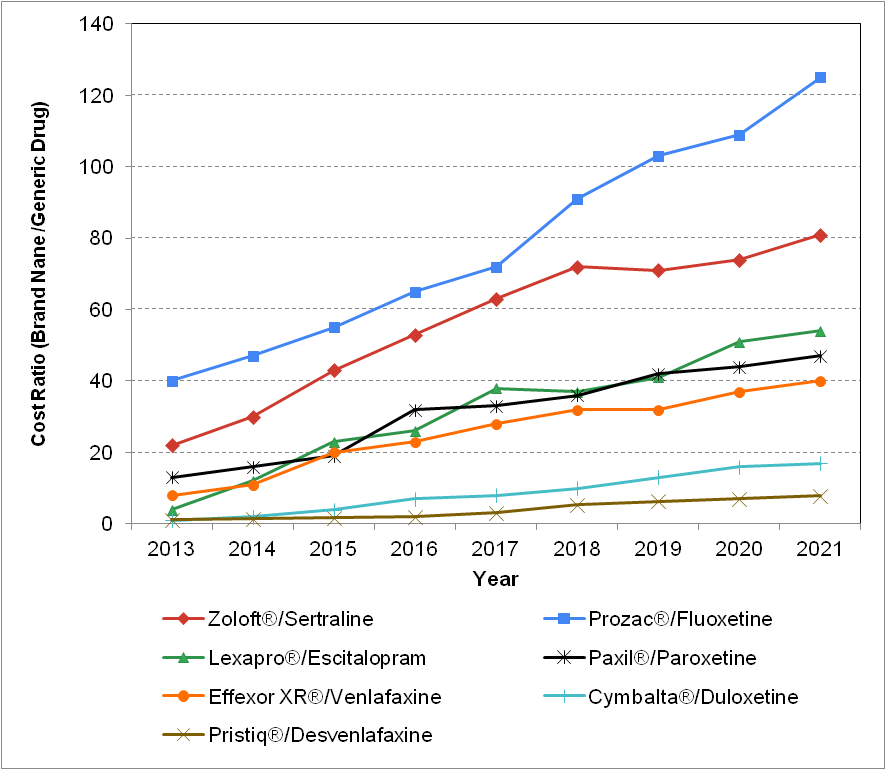
Furthermore, there has been a significant widening of the price disparity between brand-name and generic drugs. While the cost of generic drugs has shown a gradual decline over the years, brand-name pharmaceutical companies have consistently raised their prices annually. This trend is vividly depicted in Figure 3.
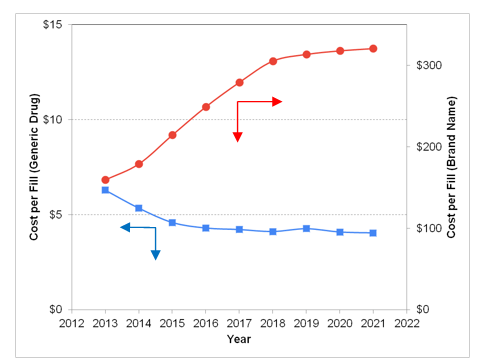
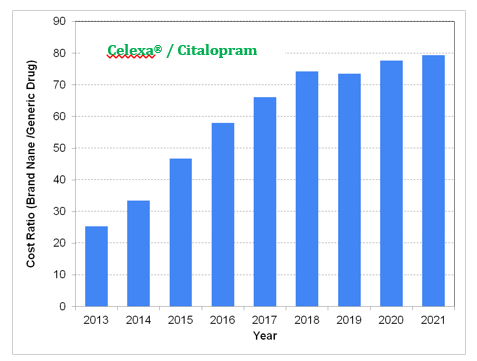
Figure 4 illustrates the evolution of the cost ratio over time, using the Celexa® / Citalopram pair as an example. In 2013, Celexa®, as a brand-name drug, was roughly 25 times more expensive than the generic Citalopram medication. However, by 2021, the cost of Celexa® has escalated to approximately 80 times that of its corresponding generic alternative.
The cost analysis for other generic/brand-name antidepressant pairs yielded consistent results, indicating the same cost trend across all pairs. As illustrated in Figure 5, the cost disparity between brand-name and generic drugs, represented by the cost ratio, has been steadily growing and becoming more substantial every year from 2013 to 2021.
This study relies on public data released by the Centers for Medicare & Medicaid Services, which encompasses aggregated data solely for Medicare Part D recipients. Although it might signify unrepresented data, the cost analysis and the trends identified remain pertinent and meaningful. Future studies that delve into different age groups could be beneficial if the cost data is accessible. Additionally, this cost-centric approach may face challenges if generic drugs do not match the tolerability and efficacy of their brand-name counterparts. Systematic analysis and comparison of reported adverse events between generic and brand-name equivalents could provide further insights in addition to this cost analysis.
4. Conclusion
In summary, the prevalence of depression appears to be increasing, particularly during the COVID-19 pandemic period. Brand-name drugs are notably more expensive than their generic equivalents, with potential savings exceeding 90% when opting for the generic version. Moreover, the cost gap between brand-name and generic medications is expanding and has become significantly more pronounced over time.
These findings underscore the critical need for enhanced monitoring and fortification of the nation's healthcare systems, especially for individuals grappling with psychiatric disorders. Administrators and policymakers could leverage this information to guide their efforts in providing not only high-quality, but also affordable care and ultimately enhancing the overall well-being of those affected by mental health conditions.
References
[1] US National Library of Medicine (2014, September 15). Mental Disorders. [Online]. Available: https://medlineplus.gov/mentaldisorders.html.
[2] S. G. Hofmann, "Toward a Cognitive-Behavioral Classification System for Mental Disorders", Behavior Therapy, vol. 45, no. 4, pp. 576-587, 2014. View Article
[3] D. Bolton, What is Mental Disorder? An Essay in Philosophy, Science, and Values, Oxford University Press, 2018.
[4] World Health Organization (2022, June 8). Mental Disorders. [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/mental-disorders.
[5] D. Telles-Correia, S. Saraiva, and J. Goncalves, "Mental Disorder - The Need for an Accurate Definition", Frontiers in Psychiatry, vol. 9, no. 64, pp. 1-5, 2018. View Article
[6] Institute of Health Metrics and Evaluation (2022, May 14). Global Health Data Exchange (GHDx). [Online]. Available: https://vizhub.healthdata.org/gbd-results/.
[7] World Health Organization (2022, June 17). WHO Highlights Urgent Need to Transform Mental Health and Mental Health Care. [Online]. Available: https://www.who.int/news/item/17-06-2022-who-highlights-urgent-need-to-transform-mental-health-and-mental-health-care.
[8] G. T. Grossberg, L. J. Kinsella (eds.), Clinical Psychophamacology for Neurologists, Springer, pp. 45-71, 2018. View Article
[9] S. B. Khushboo, "Antidepressants: Mechanism of Action, Toxicity and Possible Amelioration", Journal of Applied Biotechnology & Bioengineering, vol. 3, no. 5, pp. 437-448, 2017. View Article
[10] C. Taylor, A. D. Fricker, L. A. Devi, I. Gomes, "Mechanisms of Action of Antidepressants: From Neurotransmitter Systems to Signaling Pathways", Cellular Signalling, vol. 17, no. 5, pp. 549-557, 2005. View Article
[11] C. J. Harmer, R. S. Duman, P. J. Cowen, "How do Antidepressants Work? New Perspectives for Refining Future Treatment Approaches", Lancet Psychiatry, vol. 4, no. 5, pp. 409-418, 2017. View Article
[12] R. White (2014, January 22). Waking Up from Sadness: Many Have Trouble Getting off Antidepressants. [Online]. Available: View Article
[13] D. J. Nutt, "Relationship of Neurotransmitters to the Symptoms of Major Depressive Disorder", The Journal of Clinical Psychiatry, vol. 69, suppl. E1, pp. 4-7, 2008.
[14] N. Schimelpfening (2023, April 18). Common Antidepressant Medications. [Online]. Available: https://www.verywellmind.com/most-common-antidepressants-1066939.
[15] S. H. Preskorn, H. P. Feighner, C. Y. Stanga, R. Ross (eds.), Antidepressants: Past, Present and Future, Berlin: Springer, pp. 241-262, 2004. View Article
[16] J. R. Cashman, S. Ghirmai, "Inhibition of Serotonin and Norepinephrine Reuptake and Inhibition of Phosphodiesterase by Multi-target Inhibitors as Potential Agents for Depression", Bioorganic & Medicine Chemistry, vol. 17, no. 19, pp. 6890-6897, 2009. View Article
[17] M. S. Malvankar-Mehta, L. Feng, C. ML Hutnik, "North American Cost Analysis of Brand Name versus Generic Drugs for the Treatment of Glaucoma", ClinicoEconomics and Outcomes Research, vol. 11, pp. 789-798, 2019. View Article
[18] Health Canada (2012, April 23). The Safety and Effectiveness of Generic Durgs. [Online]. Available: View Article
[19] Centers for Medicare & Medicaid Services (2023). Medicare Part D Prescribers. [Online]. Available: View Article
[20] SDI's Vector One: National (2012, December 15). 2010 Top 200 Generic Drugs by Total Prescriptions. [Online]. Available: View Article
[21] ClinCalc (2022, October 7). Citalopram Drug Usage Statistics. [Online]. Available: View Article

