Volume 4 - Year 2017 - Pages 1-18
DOI: 10.11159/jbeb.2017.001
Knee Osteoarthritis: An Overview of Recent Interventions
Bijeet Bardoloi, Chungki Bhutia, Dinesh Bhatia*, Sudip Paul
Department of Biomedical Engineering, School of Technology,
North-Eastern Hill University, Shillong-793022, Meghalaya, India.
bijeet.bardoloi@gmail.com; bhatiadinesh@rediffmail.com; sudip.paul.bhu@gmail.com; chungkibhutia1308@gmail.com
Abstract - Knee Osteoarthritis (OA) is one of the most common forms of arthritis contributing to the burden of physical disability. This review focuses on the general and managerial aspects of knee OA. Different electrotherapeutic modalities which are commonly employed to alleviate symptoms of knee OA are Ultrasound therapy (0.5-5MHz), Transcutaneous Electrical Nerve Stimulation (2-10 Hz) and Neuromuscular Electrical Stimulation (50-100 Hz). Pulsed Electrical Stimulation (PES) is another electrotherapy treatment where low frequency current (100 Hz) is believed to promote synthesis of chondrocyte Type 2 collagen and aggrecan, and suppression of matrix metalloproteinases and Interleukin 1(IL 1), hence having a positive effect on chondrocyte function through gene regulation. In this paper, the effectiveness of electrotherapeutic modalities along with physiotherapy, surgery and other measures are reviewed. It has been found that available studies on PES have discussed limited conclusions about its role. Hence, our study aims to understand the effectiveness of PES on knee OA in comparison to commercially available technologies to overcome proposed gaps and may be treated as better therapeutic modality in near future. The data collected or conclusions drawn were through literature survey only. No experimental study or practical usage of the different devices was conducted, which could be considered in future.
Keywords: Osteoarthritis, PES, Pulsed Electrical Stimulation, Quadriceps, WOMAC.
© Copyright 2016 Authors This is an Open Access article published under the Creative Commons Attribution License terms. Unrestricted use, distribution, and reproduction in any medium are permitted, provided the original work is properly cited.
Date Received: 2016-06-27
Date Accepted: 2016-12-18
Date Published: 2017-01-05
1. Introduction
Osteoarthritis (OA) is a dynamic process and differs from simple wear and tear as it is asymmetrically distributed, often localized to only one part of a joint and associated with abnormal loading rather than frictional wear [1]. Whenever there is overwhelming imbalance between breakdown and repair of joint tissue, OA occurs [2]. Some common causes that can lead to development of OA are age related cartilage degeneration [3],[4] , genetic inheritance [5],[6], trauma, previous inflammatory conditions, quadriceps weakness[7],[8] and vascular changes [9]. One of the common joints where OA occurs is the knee. OA of the knee may be accelerated if there is a vascular disease in the subchondral bone, either through direct ischaemic effects on bone or by any alteration in the cartilage nutrition [10].
This paper is a review paper, and hence all the conclusions and inferences made were based only on literature survey. Many articles, of last twenty (20) years, related to the study were studied, compared and have been discussed. On many occasions, the results obtained from various studies done or experiments conducted have been shown and comparisons made. The advantages and disadvantages have been studied and reflected. Many studies had some limitations, which have also been shown. Overall, only study has been done on this paper and no practical or experimental study done to verify different aspects mentioned, but has been planned for in the near future.
1.1. Prevalence
OA is the commonest of all joint diseases, a true universal disorder affecting sexes and all races. However, symptoms and radiographic changes are poorly correlated in OA [11]. The burden of OA on the society is physical, psychological and socioeconomic. It can be associated with significant disability, such as a reduction in mobility and activities of day-to-day life. Psychologically distress, devalued self-worth, and loneliness are the main factors. Given the high frequency of OA in the population, its economic burden is large on the society [12]. Symptomatic knee, hand, and hip OA prevalence was significantly higher among women than men and increased significantly with age [13]. Symptomatic knee OA was also found to be significantly more common in the rural compared to urban and suburban populations [14]. In a study conducted globally, hip and knee OA ranked 11th highest contributor to global disability. The standardized global age prevalence of knee OA was 3.8% [15]. In another study, high prevalence of knee OA was found among elderly subject in Beijing, especially women, where 150 million persons age ≥60, as compared to elderly subjects in Framingham, Massachusetts [16]. In the Indian scenario, a study was conducted by M S Radha et al., 2015, to measure the prevalence of knee OA patients and identification of risk factors among the age group of 40 to 65 years in Mysore City, Karnataka and compared the Body Mass Index (BMI), Erythrocyte Sedimentation Rate (ESR) and (WOMAC) criteria. Out of 150 knee OA patients, 95 were females and 55 were males. Age group of 60-65 and 40-45 years showed the highest prevalence of knee OA, whereas the least prevalence was shown within the age group of 50-55 years. About 46% of the patients were having normal BMI and 23.33% were found to be overweight [17].
1.2. Risk factors
There are many risk factors associated with knee OA, commonly - joint dysplasia [31], intra articular fractures [18], meniscal injuries [19] etc. OA has often been found to be associated with occupation involving repetitive stress to the joint in the form of bending activities [20-21], operation of heavy vibrating tools, long term farming etc [22]. Researchers have proven that OA is more commonly seen in females than males, one of the reasons being obesity, which is more commonly seen in females [23-24]. J Dequeker et al., 1993, observed that, bone mineral density is increased, not only around the affected joints but also in generalised osteoarthritis. The change in bone mineral density is associated with a change in the mechanical properties of bone. These altered mechanical properties of the underlying subchondral bone may cause cartilage degeneration and affect the progress of disease [25]. Deborah J Hart, 1994 in his study found out that osteoarthritis and osteoporosis are inversely related, although the mechanisms remain unclear [26-27].
1.3. Pathophysiology
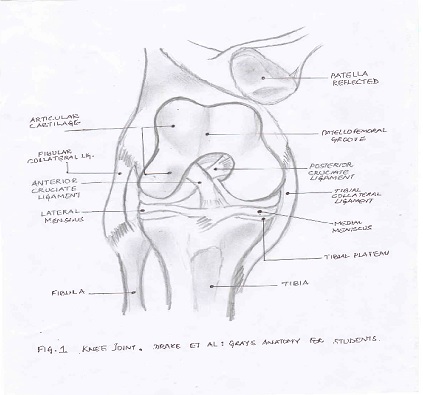
As the name suggests, pathophysiology is a convergence of pathology and physiology. It thus describes the operating mechanism of the structure and the abnormal or undesired conditions prevailing. Overall pathophysiology explains the mechanisms whereby such conditions develop and progresses. In the case of a normal knee joint, it consists of femoropatellar articulation, which consists of the knee cap known as patella and patellar groove, medial and lateral femorotibial articulations linking the femur with the tibia [28]. For the smooth sliding of the bones, cartilage tissues, which are of two types - meniscus and hyaline cartilage, are present. It is the cartilage that wears out eventually. The menisci protect the bones from rubbing on each other and also help in shock absorption. Along with the menisci, ligaments help in protection of the joint [29-30]. Figure 1 shows all the above mentioned parts of the normal knee joint. Abnormal joint loading is a major reason for the development of knee OA. Disparity between the joint load and the ability to cope up with the stress causes the destruction of cartilage along with other factors. Mechanical and enzymatic factors are thought to impair chondrocyte function and damage the cartilaginous matrix [31].
2. Diagnosis
Though the effects of OA can show up during later stages of life, the onset of the process can be quite early. Early detection can help a lot to prolong the process. If diagnosis is done at an earlier stage, proper measures can be taken to improve the conditions. The major elements of the diagnostic evaluation are the history, physical examination, imaging studies, and, in some cases where special questions arise, laboratory testing is employed.
2.1. History and Physical Examination
The criteria laid down by the American College of Rheumatology (ACR) are widely followed in the diagnosis of OA. They are, knee pain, radiographic osteophytes and at least 1 of the following 3 items: Age >50 years, morning stiffness of 30 minutes or less and crepitus on motion [32]. The physical examination of the knee ligaments consists of testing of the lateral ligaments with the varus or valgus stress test [33-34] and testing of the anterior and posterior cruciate ligaments with the drawer test [35]. Likewise, the menisci should be diagnostically tested manually using Apley compression test [36] and McMurray test [37]. The patella-femoral joint is assessed by employing test like Zohlens [38].
2.2. Imaging Studies
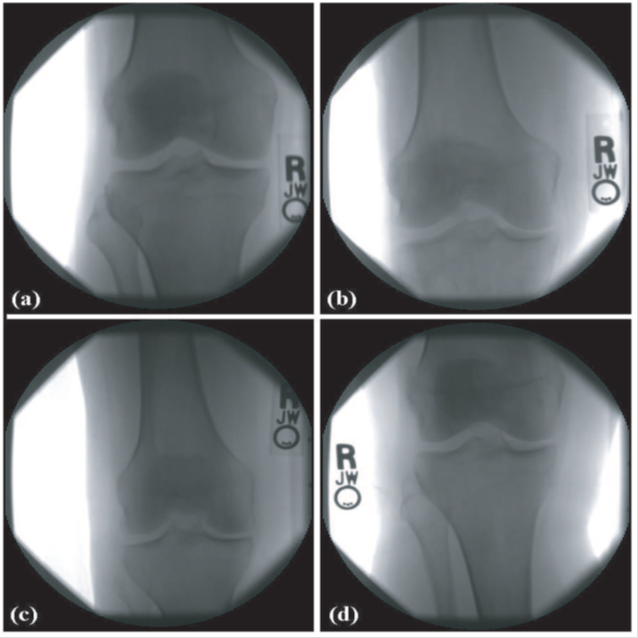
Despite the development of newer imaging techniques, the radiograph remains the most accessible tool in the evaluation of the OA joint. X-ray imaging studies are used both for primary diagnosis and to assess the progression of the disease. The typical radiological signs of knee osteoarthritis that can be seen on plain films are incorporated in the staging system of Kellgren and Lawrence [39-41]. The staging of osteoarthritis of the knee, after Kellgren and Lawrence scale can be classified as: Stage 0(no abnormality), Stage 1(incipient osteoarthritis, beginning of osteophyte formation on eminences), Stage 2( moderate joint space narrowing, moderate subchondral sclerosis), Stage 3( >50% joint space narrowing, rounded femoral condyle, extensive subchondral sclerosis, extensive osteophyte formation), Stage 4(joint destruction, obliterated joint space, subchondral cysts in the tibial head and femoral condyle, subluxed position), as shown in figure 2. Others forms of imaging are Magnetic Resonance and Imaging (MRI), which helps to detect cartilage defects and bone marrow lesions [42-43], Optical coherence tomography (OCT) which can demonstrate real-time imaging in vivo of human cartilage at a resolution of micrometers [44] and Scintigraphy which can predict subsequent loss of joint space in patients with established OA of the knee joint [45] etc.
3. Management of Knee Osteoarthritis
Osteoarthritis (OA) is not a curable disease at present, as the mechanism by which it arises and progresses remains incompletely understood. Therefore, the goal of treatment is to alleviate the signs and symptoms of the disease and, if possible, to slow its progression. The therapeutic spectrum ranges from general measures to physiotherapy, orthopaedic aids and orthosis, pharmacotherapy, and finally surgery and rehabilitation. The goals of treatment, as stated in many of the guidelines are: pain relief, improve quality of life, improve mobility, improve walking and delay progression of osteoarthritis.
3.1. General measures
Some general measures for reducing chances of OA occurrence are patient education, lifestyle adjustment, and, when indicated, weight loss. Chodosh et al., 2005, in a meta-analysis, found that general measures have no appreciable effect on pain and function in knee osteoarthritis [46]. A further meta-analysis of 16 controlled trials yielded the finding that individual exercise and self-management had a moderate, but clinically significant psychological effect and made a positive contribution to the patients' emotional well-being [47]. In one study, R. Christensen et al., 2005, found out that, 8 weeks of Low Energy Diet (3.4 MJ/day) was found to be advantageous because of the rapidity of weight loss and a more significant loss of body fat [48]. In some cases, elderly patients diagnosed with knee OA are apprehensive about exercising. In one study, it has been found that, provided trauma is avoided, moderate exercise does not lead to acceleration of knee osteoarthritis, whether or not there is evidence of pre-existing disease. It is likely that exercise interventions are underused in the management of established knee OA symptoms [49-50]. Usage of cane can diminish pain, improve function and some aspects of quality of life in patients diagnosed with knee OA [51].
3.2. Orthopaedic Aids and Orthosis
Brouwer RW et al., 2005, conducted a study to evaluate the effect of a brace intended to reduce load in patients with medial or lateral compartmental osteoarthritis and concurrent varus or valgus alignment, respectively. They found out that a brace intended to reduce load shows small effects in patients with unicompartmental osteoarthritis. However, many patients do not adhere in the long run to this kind of conservative treatment [52].
3.3. Pharmacotherapy
One of the procedures to be followed for management of knee OA is pharmacotherapy. In this procedure, usage of medicines or drugs is employed. It is generally used to relieve the patient from pain and inflammation. The following classes of medications are currently used to treat osteoarthritis of the knee: analgesics/anti-inflammatory agents, glucocorticoids, opioids, symptomatic, slow-acting drugs for osteoarthritis (SYSADOA) and anti-cytokines [53]. Research studies have showed that though Cochrane database contains a review of 16 randomized trials, yet, despite the large number of studies the efficacy and safety of these drugs cannot yet be judged conclusively [54]. When signs of inflammation arise, intraarticular glucocorticoid injections can rapidly eliminate a joint effusion. The most suitable type of glucocorticoid for injection has been found to be one with a long half-life, in crystalloid solution, with a small crystal size e.g. triamcinolone acetonide or hexacetonide, at a dose of 10 mg or 40 mg, respectively. A number of studies have shown that intra-articular corticosteroids (IAS) injections are effective than hyaluronic acid (HA), placebo or lavage [55-57]. However, in some cases septic arthritis has emerged as a serious potential complication from repeated intra-articular injections [58]. Towheed et al., 2005, found that Slow Acting Drugs for OA slow the radiological progression of knee osteoarthritis [59]. It was shown that either high or low molecular weight use of HA was effective in improving WOMAC pain and function scores than using IAS or intra-articular placebo (IAP). Hence, the American Medical Society for Sports medicine (AMSSM) recommends the use of HA for the appropriate patients suffering from knee OA [60-61]. Osteoarthritis Research Society International (OARSI) members recommended the use of 25 different modalities. The eight recommendations covering pharmacological modalities of treatment includes acetaminophen, cyclooxygenase-2 (COX-2) non-selective and selective oral nonsteroidal anti-inflammatory drugs (NSAIDs), topical NSAIDs and capsaicin, intraarticular injections of corticosteroids and hyaluronates, glucosamine and/or chondroitin sulphate [62] for symptom relief; glucosamine sulphate, chondroitin sulphate and diacerein for possible structure-modifying effects and the use of opioid analgesics for the treatment of refractory pain. OARSI recommendations for the management of hip and knee OA, states that overall there was no statistically significant difference between non-pharmacological therapies and pharmacological therapies. However, optimal management of patients with OA hip or knee requires a combination of nonpharmacological and pharmacological modalities of therapy [63]. In most cases, OA patients find usage of NSAIDS more effective than acetaminophen. However in one study, researchers have found that the efficacy of ACET, 1000 mg four times a day, on average, was found effective than that of either an analgesic or an anti-concluding that adequate relief of osteoarthritic pain could be achieved in some cases with an analgesic [64-65]. On a debate whether older patients with chronic knee pain should be advised to use topical or oral non-steroidal anti-inflammatory drugs, researchers concluded that, both have same effectiveness, but usage of oral NSAIDS could have gastrointestinal (GI) side effects, hence topical use is preferred by elderly patients with knee OA [66]. ACR has recommended a set of 'strong' and 'conditional' recommendations for use of non-pharmacological and pharmacological therapies, for patients suffering from knee OA. Non-pharmacological modalities strongly recommended for the management of knee OA were aerobic, aquatic, and/or resistance exercises as well as weight loss for overweight patients. Non-pharmacologic modalities conditionally recommended for knee OA included medial wedge insoles for valgus knee OA, subtalar strapped lateralinsoles for varus knee OA, medially directed patellar taping, manual therapy, walking aids, thermal agents, tai chi, self-management programs, and psychosocial interventions. Pharmacologic modalities conditionally recommended for the initial management of patients with knee OA included acetaminophen, oral and topical NSAIDs, tramadol, and intra-articular corticosteroid injections; intra-articular hyaluronate injections, duloxetine, and opioids were conditionally recommended in patients who had an inadequate response to initial therapy. Opioid analgesics were strongly recommended in patients who were either not willing to undergo or had contraindications for total joint arthroplasty after having failed medical therapy [67].
3.4. Surgery
Five surgical modalities that are recommended by OARSI are; total joint replacements, unicompartmental knee replacement, osteotomy and joint preserving surgical procedures; joint lavage [68] and arthroscopic debridement in knee OA, and joint fusion as a salvage procedure when joint replacement had failed. A study conducted by Sylvia et al., 2012, showed that patients diagnosed with non-traumatic degenerative meniscal tear when treated with combination of arthroscopy and exercise or exercise alone, both showed significant clinical improvement from the baseline to the follow ups at 24 and 60 months. However later, one third of the patients in the exercise alone group started showing symptoms and thus had to undergo arthroscopy treatment. The findings indicate that arthroscopic surgery followed by exercise therapy was not superior to the same exercise therapy alone for this type of patients [69]. On one study to find out the efficacy of arthroscopic surgery for the treatment of osteoarthritis of the knee, the researchers found out that Arthroscopic surgery for osteoarthritis of the knee provides no additional benefit to optimized physical and medical therapy [70]. The goal of bone stimulating techniques is to open the subchondral cartilage and thereby bring pluripotential stem cells to the joint surface, where they are then supposed to form fiber bundles under the influence of mechanical and biological forces. Studies have not revealed any significant differences between the various methods that are used [71]. In Autologous chondrocyte transplantation cartilage cells are taken from the joint, enzymatically isolated and cultured ex vivo, and then put back into the joint at the site of the cartilage defect, which is prepared before the cultured cells are added [72]. Long term results are not yet available to document the survival of implanted cartilage cells [73]. In Autologous osteochondral transplantation (OCT), mosaicplasty, cylinders of cartilage and bone are taken from a part of the joint that is not affected, and then inserted into the cartilage defect with press-fit technology. In principle, OCT can be performed through an arthroscope, unless the defect is too large [74]. The reported results of OCT are, in general, very promising [75]. Corrective osteotomy, either tibial osteotomy or femoral osteotomy is carried out to relieve pain in osteoarthritic knee which has either varus or valgus deformity [76]. As shown by Petterson, 2006, total knee replacement is one of the most sought after option in cases of end stage arthritis. Total knee replacement by modern technologies promises improvement lasting 15 years or longer. However these operations are very expensive, highly dependent on technical skills and the kind of implant materials employed [77].
3.5. Physiotherapeutic Measures
Physiotherapy for knee osteoarthritis includes exercise therapy as well as electrotherapy including ultrasound application, Transcutaneous Electrical Nerve Stimulation (TENS), muscle stimulation, Pulsed electrical stimulation (PES) etc. Ultrasound (US) refers to mechanical vibrations which are similar to sound waves but of a higher frequency. The frequency employed for physiotherapeutic purposes is in the range from 0.5 to 5 MHz. Piezoelectrical transducers are used to achieve the high frequency ultrasound energy needed for imaging and therapy. These are suitably cut crystals (quartz, barium titanate or lead zirconate titanate) which change shape under the influence of an electric charge. The other essential parts of therapeutic ultrasound generator are a circuit to produce oscillating voltages to drive the transducer and a controlling unit which can turn the oscillator on and off to give a pulsed output. The principle therapeutic uses of ultrasound include promoting the healing of chronic ulcers, healing of acute soft tissue injuries, relief of both neurogenic and chronic pain, improvement of scar tissue etc [78]. Table 1 shows some recent study of US therapy for management of knee OA.
Table 1. Recent study of US therapy for management of knee OA.
| Year | Author | Research/Work | Achievement/Outcome | Limitations |
| 1995 | Arne Nyholm Gam et al [95] | A meta-analysis of 293 papers published since 1950 to assess the evidence of effect of US in the treatment of musculoskeletal disorders. | Pain relief could not be achieved by ultrasound treatment hence, they concluded that the use of ultrasound in treatment of musculoskeletal disorders is based on empirical experience | Study is lacking firm evidence from well-designed controlled studies |
| 1999 | Danielle A.W.M. van der Windt et al [96] | Study to evaluate the effectiveness of US therapy in the treatment of musculoskeletal disorders. | No statistical significant outcome in favor of US therapy | Little evidence to support the use of US therapy in the treatment of musculoskeletal disorders |
| 2005 | Judith Falconer et al [97] | An RCT to determine the effectiveness of US (plus exercise) in relieving stiffness and pain on 69 patients diagnosed with knee OA and chronic knee contracture. | Study showed that both groups significantly improved in active ROM, pain, and gait velocity, and maintained improvement for at least 2 months. | Benefits of exercise program may have led to improvement in range of motion. |
| 2007 | Rita A Wong et al [98] | Survey study on 457 physical therapists (orthopedic certified specialists from the Northeast/Mid-Atlantic regions of the United States). | The respondents indicated that they were likely to use US for patient treatment. Thus Ultrasound continues to be a popular adjunctive modality in orthopedic physical therapy. | These findings may help researchers prioritize needs for future research on the clinical effectiveness of US |
| 2008 | Cetin N et al [99] | Study to understand the effectiveness of application of US and hot packs prior to isokinetic exercises on patients with bilateral knee OA | Improvement in isokinetic performance as well as physical function seen in treatment groups. | None reported |
| 2008 | Levent Özgönenel et al [100] | A randomized double blind clinical trial on 67 patients to determine the effectiveness of US therapy in knee OA | Statistically significant improvement was seen in the experimental group as compared to the placebo group. | None reported |
| 2008 | GroJamtvedt et al [101] | Systematic reviews published between 2000 and 2007 on physical therapy interventions for patients with knee OA | Besides exercises, weight reduction, acupuncture, TENS and low level laser therapy, the quality of evidence is low in other interventions incorporated in the treatment of knee OA. | None reported |
| 2008 | John Z Srbely et al [102] | A Pubmed search of the literature was performed from 1985 to 2008 and retrieved a total of 313 publications. A total of 17 articles met the researchers search criteria and hence was considered. | Ultrasound proven to therapeutically beneficial, safe and effective for the management of knee OA | Lack of consistency in current literature. Strict methodologies and meticulous reporting of output parameters and application techniques mandate in future studies. Conduct of isolated studies on US alone by excluding adjunctive modalities in their methodology. |
| 2010 | F Tascioglu et al [103] | A study to understand the effectiveness of either pulsed US, continuous US or sham US on 90 patients with idiopathic knee OA aged 54 - 70 years. | pulsed ultrasound therapy was proven to be safe and effective form of treatment modality | Long term efficacy of ultrasound therapy for knee OA requires further investigation. |
| 2010 | A. Loyola-Sánchez et al [104] | A systematic review of US therapy on knee OA | US could be efficacious for decreasing pain and may improve physical function in patients with knee OA | Low quality of evidence. More clinical trials are mandate. |
| 2010 | Rutjes AWS et al [105] | Study on effectiveness of US therapy on knee or hip OA when compared to sham treatment or no treatment. | Therapeutic ultrasound may be beneficial for patients with osteoarthritis of the knee | Methodological quality and the quality of reporting was poor and a high degree of heterogeneity among the trials was revealed for knee function |
| 2013 | Mirsad Muftic et al [106] | Prospective study on 68 patients to determine the effectiveness of continuous US to chronic musculoskeletal pain. | Chronic pain caused by degenerative changes could be alleviated by application of continuous ultrasound. | None reported |
Conclusions drawn from the table showed that besides a few studies where no significant changes were observed, other studies showed significant improvement and was found to be beneficial as it was safe and improvement in physical functions in patients were observed with reduction in pain.
Transcutaneous Electrical Nerve Stimulation (TENS) is the application of low frequency current in the form of pulsed rectangular current through surface electrodes. TENS is usually employed for pain relief. TENS is mostly applied as short pulses of around 50micro seconds at 40-150 Hertz, called as conventional TENS, and is a high frequency, low intensity stimulation. These low intensity short pulses will selectively stimulate the large low threshold A Beta fibres and produce pain inhibition by pain gate mechanism, as proposed by Melzac and Wall, 1965 [79]-80]. This conventional mode is the most usual method for self-treatment. The recommended duration and timing of such treatment varies from 30-60 minutes sessions, once or twice a day as stated by Klein and Pariser, 1987 [81].
Acupuncture like TENS or high intensity, low frequency stimulation, is commonly used. Pulses of around 0.2 milli seconds at about 2 Hertz are given at intensities so that a visible contraction can be seen. This kind of stimulation stimulates the small diameter A delta and C fibres causing release of endogenous opioids. It is mostly applied to acupuncture points hence relieving pain. It is applied for 20-30 minutes per session.
Table 2 shows an overview of some recent study on TENS therapy on knee OA. There have been a few contradictory results. Though there have been inconclusive results, many results concluded that it was effective only for a short term duration, and that too mostly pain relief.
Table 2. Recent study on TENS therapy for management of knee OA.
| Year | Author | Research/Work | Achievement/Outcome | Limitations |
| 2001 | Osiri et al [107] | Systemic review of TENS on knee osteoarthritis | Conventional TENS and acupuncture-like TENS effective over placebo | The studies were heterogeneous with different study designs and outcomes used |
| 2003 | Kathleen A. Sluka and Deirdre Walsh [108] | Study of clinical effectiveness of TENS. | Though TENS is a non-invasive modality that is easy to apply, clinical efficacy remains equivocal | Sufficient numbers of high quality, randomized, controlled clinical trials needs to be done |
| 2003 | Gladys L. Y. Cheing et al [109] | Study to examine the optimal stimulation duration of TENS for relieving OA knee pain and the duration of post-stimulation analgesia | 40 mins is the optimal treatment duration of TENS, in terms of both the magnitude of pain reduction and the duration of post-stimulation analgesia for knee OA | 28 patients received either 20 mins, 40 mins, 60 mins of TENS or 60 mins of placebo TENS 5 days a week for 2 weeks |
| 2004 | Pearl P. W. Law et al [110] | Study on the improvement of physical performance of people with knee OA using TENS | Improvement observed till about 10 days, insignificant beyond it | A larger study with the assessment of other functional outcomes may be required |
| 2007 | Kazunori Itoh et al [111] | Study tests whether a combined treatment of acupuncture and TENS is more effective than acupuncture or TENS alone for treating knee osteoarthritis (OA). | The study showed that TENS gave short relief from pain while acupuncture gave a longer relief and the combination of both gave a better result than control group, only acupuncture or only TENS treatments. | Initially 32 patients were taken for the purpose, but on completion, only 24 remained. |
| 2007 | Jan M Bjordal et al [112] | Assessment of the short-term pain relief of the physical agents for knee osteoarthritis | 2-4 week treatment regime seemed to offer clinically relevant short-term pain relief | No. of trials taken were 11 |
| 2009 | Anne W.S. Rutjes et al [113] | Comparison of TENS with sham or no specific intervention in terms of effects on pain and withdrawals due to adverse events in patients with knee osteoarthritis | The study was inconclusive. It could not be confirmed that TENS was effective for pain relief | Small trials of questionable quality. Appropriately designed trails of adequate power were warranted |
| 2012 | Wright A. [114] | A study to explore the evidence for using TENS to relieve pain | Literature available provides conflicting evidence. | Inherent problems with trail designs. |
| 2015 | Carol G.T. Vance et al [115] | Critical review of the latest basic science and clinical evidence for TENS | High frequency and low frequency TENS have been shown to provide analgesia specifically when applied at a strong, non-painful intensity and high frequency TENS may be more effective for people taking opioids. | Further investigation is warranted to ensure optimal use. Investigation in the area of TENS tolerance is necessary |
Electrical stimulation has been used to increase strength [82] and endurance of muscle, improve range of motion, neuromuscular re-education, pain management, reducing oedema, and as an aid in the healing of bone fractures and pressure sores. Electrical stimulation excites the motor nerve going to muscle and not muscle itself. Therefore, high frequency stimulation (>70 Hz) may cause neuromuscular junction failure and muscle will rapidly fatigue. The optimum frequency is similar to the range of normal motor unit discharge frequencies generated during voluntary activity, 20-50 Hz. Lower frequencies cause an unfused muscle contraction. With optimum electrical stimulation, the cutaneous sensory nerves gets stimulated first, followed by motor nerve stimulation and finally the stimulation of small diameter pain fibres. The sequence of stimulation of these three types of nerve fibers is affected in the same order with any form of stimulating pulse. Neuromuscular electrical stimulation (NMES), used interchangeably with electrical stimulation (ES), is typically provided at higher frequencies (20-50 Hz) to produce muscle tetany and contraction that can be used for functional purposes. Some recent studies on NMES therapy for knee OA management have been shown in table 3.
Table 3. Recent study on NMES therapy for management of knee OA.
| Year | Author | Research/Work | Achievement/Outcome | Limitations |
| 1992 | David A. Lake [116] | An overview of the effects of NMES and its application on sports injuries | NMES can improve functional performance in a variety of tasks. NMES has been shown to be effective in preventing the decrease in muscle strength, muscle mass and the oxidative capacity of thigh muscles | Unclear whether the selective strengthening is due to local changes in muscle or to a change in the relative magnitude of recruitment of the different muscles |
| 2005 | John P. Porcari et al [117] | To study the effects of self administered NMES on the abdominal wall to check changes in strength, endurance, selected anthropometric measures and subject's perceived shape | The study found that NMES significantly increased the isometric strength and dynamic endurance of the abdominal musculature. | Studies may be needed to compare the benefits of using NMES to those performing abdominal curls |
| 2010 | Palmieri-Smith et al [118] | Study to determine whether NMES is capable of improving quadriceps muscle strength and activation in women with mild and moderate knee OA | Improvement was not realised. | Women were enrolled based on radiographic evidence of OA, not symptomatic. Also assessor and patients were not blinded to group assignment |
| 2011 | Julien Gondin et al [119] | To provide an overview on the benefits and limitations of NMES training program in healthy individuals and in recreational and competitive athletes regarding muscle performance | Short term NMES training appears as an attractive tool for increasing muscle performance. It imposes a specific muscle stress leading to the recruitment of motor units different from those activated throughout voluntary actions | Future studies should focus on the chronic effects of NMES. Also it is needed to better understand the influence of reduced NMES training volume |
| 2012 | Bruce-Brand et al [120] | Comparison of NMES, resistance training (RT) and standard care in subjects with moderate to severe knee OA | NMES program significantly improves functional performance in patients with moderate to severe OA. Significant intra-group increase in quadriceps CSA | Dose-response studies with longer follow-up are required to establish the optimum frequency and intensity on NMES training |
| 2012 | Marco Aurélio Vaz et al [122] | Identifying the association of knee OA with quadriceps muscle architecture and strength and quantifying the effects of a NMES training program on these parameters | Knee OA patients have decreased strength, muscle thickness and fascicle length compared to age and sex matched controls. NMES training offset the changes of quadriceps structure and function, reduces joint pain and stiffness and functional limitation | How NMES reduces muscle inhibition is not clear. The possibility that after NMES training, strength gains observed may partly be associated with an improvement in activation capacity of the quadriceps, needs to be further investigated |
| 2013 | Aline Mizusaki Imoto et al [123] | The study investigated the effect of 8 weeks of NMES + Ex (Exercise) on pain and functional improvement in patients with knee OA compared to Ex alone | The addition of NMES to Ex did not improve the outcomes assessed in knee OA patients | 100 no. of patients were taken into consideration (86 women and 14 men) with age ranging from 50 to 75 years |
Results obtained from the table showed no improvement in two cases whereas in almost all the cases, significant increase in muscle strength was observed, hence increase in functional performance in patients.
One electrotherapy treatment technique, namely the pulsed electrical stimulation (PES), has been employed to decrease pain and improve function in knee OA. High Voltage PES has shown to retard edema formation in an experiment done on golden hamsters [83], and in some cases have caused healing of dermal ulcers [84]. However, there are not much supported literature available showing the use of PES in the management of OA. Some recent studies on PES therapy used for the management of knee OA have been shown in table 4.
Table 4. Recent study on PES therapy for management of knee OA.
| Year | Author | Research/Work | Achievement/Outcome | Limitations |
| 1995 | Thomas M Zizic et al [124] | Prospective, randomized, placebo controlled double blind study to test the effectiveness of PES device (Bionicare Stimulator, Model BIO-1000TM ) on patients with knee OA | Intermittent PES therapy provided significant short term improvement in knee pain, function, knee flexion, and duration of morning stiffness in patients with knee OA. | Treatment time was only for four weeks. |
| 2006 | Farr J et al [125] | Prospective cohort study on 288 patients to see the effectiveness of PES on knee pain n other symptoms. | This study showed that use of PES device can reduce knee OA symptoms in patients who had failed non surgical treatment. | None reported |
| 2007 | D. Garland et al [126] | A 3-month, double-blind, placebo-controlled trial, using either an active (BIO 1000 TM BioniCare Medical Technologies Inc ) or placebo device at home on patients with knee OA | Improvement in symptoms and functions in knee OA without any serious side effects. | None reported |
| 2009 | Robyn E Fary et al [127] | Case study on three subjects with knee OA to see the effectivesness of PES device(BIO 1000TM, BioniCare Technologies) | Improvement on all outcomes were seen on two patients , but not so significant improvement was seen on one patient | Longer randomized controlled studies are needed to understand the effectiveness of Pulsed electrical stimulation. |
| 2011 | Robyn E. Fary et al [128] | A double-blind, randomized, placebo-controlled, repeated-measures trial , in 70 patients diagnosed with knee OA of the knee who were randomized to either PES or placebo group. | No significant improvement in the experimental group as compared to the placebo group. | Less literature available |
| 2013 | A. Negm et al [129] | To understand the effectiveness of low frequency (<100Hz) subsensory stimulation produced either by using Pulsed electromagnetic field(PEMF) or PES on knee pain and physical function of patients suffering from knee OA | Low frequency stimulation was effective in improving physical function but not pain intensity. | Inconclusive results due to less number of literatures available. More studies are mandate to confirm the findings of this systematic review. |
| 1995 | Thomas M Zizic et al [124] | Prospective, randomized, placebo controlled double blind study to test the effectiveness of PES device (Bionicare Stimulator, Model BIO-1000TM ) on patients with knee OA | Intermittent PES therapy provided significant short term improvement in knee pain, function, knee flexion, and duration of morning stiffness in patients with knee OA. | Treatment time was only for four weeks. |
| 2006 | Farr J et al [125] | Prospective cohort study on 288 patients to see the effectiveness of PES on knee pain n other symptoms. | This study showed that use of PES device can reduce knee OA symptoms in patients who had failed non surgical treatment. | None reported |
From table 4, it can be seen that PES is a very recent method of physiotherapeutic intervention, and hence limited research works were found on it. The literature survey conducted with a few research works showed that the study was either of short duration, no improvement shown or number of subjects was less. A few studies did show some improvements regarding OA symptoms. Hence further research needs to be done in this area.
Application of PES affects the cartilaginous tissue, not all electric field or stimuli affect the cartilage. The effect on the cartilage depends on many factors, namely field strength, frequency, wave-form, time and duration of application etc.
Experiments performed with PES showed capacitively combined electric field increased glycosaminoglycan synthesis and chondrocyte cell proliferation in calf hyaline cartilage pellets and time-varying electrical fields could heal total thickness cartilage lesions with hyaline cartilage in a rabbit model of osteoarthritis. In another experiment, it was seen that electrical stimulation when added to background NSAIDs or analgesics enhanced pain reduction and increased function. Thus, in vitro, animal histological and human data exist to support further trials of time-varying electrical stimulation in human osteoarthritis [145].
4. EMG studies on OA knee
Electromyography (EMG) is an experimental technique concerned with the development, recording and analysis of myoelectric signals [130]. Till date; EMG signals have been used for better understanding and diagnosis of various diseases [141-143], evaluation of different exercises [144], understanding of muscle function [134], neuromuscular pattern [139], and estimation of muscle forces [131]. In one such study conducted by David G. Lloyd et al, 2003, an EMG driven musculoskeletal model of the human knee was employed to predict knee moments in different dynamic contractile conditions [132]. EMG study has also been employed to provide knowledge about the dominant force producing muscle during a particular test procedure in the lower extremity [133]. Ozlem O. Yilmaz et al, 2010, have shown that there is no significant superiority of EMG-biofeedback-assisted strengthening exercise program to strengthening exercise program without EMG-biofeedback, however there was improvements in parameters such as muscle strength, pain and function in both the groups after the treatment [137].
Disturbances in normal load distribution and altered muscle activity have been associated with knee OA which can cause further deterioration of the knee joint. Tibor Hortobágyi et al., 2005, found that there is increased hamstring muscle activation than the quadriceps group [138], while performing routine daily tasks in subjects with knee OA. Hence, it has been observed that patients with knee OA have higher antagonist muscle activity [140] as compared with the control subjects.
5. Conclusion
Knee OA is considered to be the fourth highest cause of disability in women and is responsible for the deterioration of quality of life and functional capacity [85]. A plethora of studies have investigated several aspects related to muscle function, such as aerobic capacity [86], muscle strength [87] as well as other clinical aspects such as pain [88], Range of Motion [89], stiffness [90], and WOMAC Index [91] in patients suffering from knee OA. However there are scant Electromyogram (EMG) studies for those diagnosed with moderate and severe OA [92]-[94]. This review has certain limitations. Since only English language articles were included, it is possible that this review is not a complete representation of the available evidence. The review was limited to published articles and thus may have missed those that were not submitted or accepted for publication, presenting a possible publication bias. We are conducting an in house study employing EMG and motion studies to understand the muscle activities, kinematics and dynamics around knee joints of those patients suffering from moderate to severe knee OA. The study shall be age and gender controlled study. Simultaneous study of ground reaction forces on the affected limb shall be conducted to understand the loading on knee joint, while the subject performs routine daily tasks. We aim to utilize these results in the development of a pulsed electrical knee stimulator for relief of knee symptoms.
6. Acknowledgements
We would like to acknowledge the support of the Department of Science and Technology, Government of India, for funding the study entitled "Design of Pulsed Electrical knee Stimulator for Osteoarthritis patients" [ Ref No.: DST NO: IDP/MED/31/2013]. We also acknowledge the support of all the volunteers enrolled for the study and Orthopaedics Department at North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences NEIGRIHMS, Shillong.
References
[1] L. Solomon, D. Warwick and S. Nayagam, Apley's system of orthopaedics and fractures, 9th ed., CRC press, 2010. View Book
[2] D. J. Hunter, J. J. McDougall and F. J. Keefe, "The symptoms of osteoarthritis and the genesis of pain," Med Clin North Am, vol. 93, no. 1, pp. 83-100, 2009. View Article
[3] P. D. Byers, F. T. Hoaglund, G. S. Purewal and A. C. Yau, "Articular cartilage changes in Caucasian and Asian hip joints," Ann rheum Dis, vol. 33, no. 2, pp. 157-161, 1974. View Article
[4] M. V. Foss and P. D. Byers, "Bone density, osteoarthrosis of the hip, and fracture of the upper end of the femur," Ann Rheum Dis, vol. 31, no. 4, pp. 259-264, 1972. View Article
[5] J. H. Kellgren, J. S. Lawrence and F. Bier, "Genetic factors in generalized osteoarthrosis," Ann Rheum Dis, vol. 22, pp. 237-255, 1963. View Article
[6] R. G. Knowlton, E. J. Weaver, A. F. Struyk, W. H. Knobloch and R. A. King, et al, "Genetic linkage analysis of hereditary arthro-ophthalmopathy (Stickler syndrome) and the type II procollagen gene," Am J Hum Genet, vol. 45, no. 5, pp. 681-688, 1989. View Article
[7] S. C. O'Reilly, A. Jones, K. R. Muir and M. Doherty, "Quadriceps weakness in knee osteoarthritis: the effect on pain and disability," Ann Rheum Dis, vol. 57, p. 588-594, 1998. View Article
[8] M. D. Lewek, K. S. Rudolph and L. Snyder-Mackler, "Quadriceps Femoris muscle weakness and activation failure in patients with symptomatic knee osteoarthritis," J Orthop Res, vol. 22, no. 1, p. 110-115, 2004. View Article
[9] M. H. Harrison, F. Schajowicz and J. Trueta, "Osteoarthrits of the hip: a study of the nature and evolution of the disease," J Bone Joint Surj Br, vol. 35, pp. 598-626, 1953. View Article
[10] S. Zhou, Z. Cui and J. P. Urban, "Factors influencing the oxygen concentration gradient from the synovial surface of articular cartilage to the cartilage-bone interface: a modeling study," Arthritis Rheum, vol. 50, no. 12, pp. 3915-3924, 2004. View Article
[11] J. Ledingham, M. Regan, A. Jones and M. Doherty, "Radiographic patterns and association of osteoarthritis of knee in patients referred to hospital," Ann Rheum Dis, vol. 52, pp. 520-526, 1993. View Article
[12] A. Litwic, M. H. Edwards, E. M. Dennison and C. Cooper, "Epidemiology and burden of Osteoarthritis," Br Med Bull, vol. 105, p. 185-199, 2013. View Article
[13] J. L. Van Saase, L. K. Van Romunde, A. R. Cats, J. P. Vandenbroucke and H. A. Valkenburg, "Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations," Ann Rheum Dis, vol. 48, no. 4, pp. 271-280, 1989. View Article
[14] A. A. Andrianakos, L. K. Kontelis, D. G. Karamitsos, S. I. Aslanidis, A. I. Georgountzos and G. O. Kaziolas, et al, "ESORDIG Study Group. Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece," The ESORDIG study. J Rheumatology, vol. 33, no. 12, pp. 2507-2513, 2006. View Article
[15] M. Cross, E. Smith, D. Hoy, S. Nolte, I. Ackerman and M. Fransen, et al, "The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study," Ann Rheum Dis, 2010. View Article
[16] Y. Zhang, L. Xu, M. C. Nevitt, P. Aliabadi, W. Yu, M. Qin, L. Y. Lui and D. T. Felson, "Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: The Beijing Osteoarthritis Study," Arthritis & Rheumatism, vol. 44, no. 9, pp. 2065-2071, 2001. View Article
[17] M. S. Radha and M. R. Gangadhar, "Prevalence of knee osteoarthritis patients in Mysore city, Karnataka," Int J Recent Sci Res, vol. 6, no. 4, pp. 3316-3320, 2015. View Article
[18] T. C. Merchant and F. R. Dietz, "Long-term follow-up after fractures of the tibial and fibular shafts," J Bone Joint Surg Am, vol. 71, no. 4, pp. 599 -606, 1989. View Article
[19] B. E. Øiestad, L. Engebretsen, K. Storheim and M. A. Risberg, "Knee osteoarthritis after anterior cruciate ligament injury a systematic review," Am J Sports Med, vol. 37, no. 7, pp. 1434-1443, 2009. View Article
[20] D. T. Felson, M. T. Hannan, A. Naimark, J. Berkeley, G. Gordon, P. W. Wilson and e. al, "Occupational physical demands, knee bending, and knee osteoarthritis: results from the Framingham Study," J Rheumatol, vol. 18, no. 10, pp. 1587-1592, 1991. View Article
[21] D. Cogon, S. Kellingray, H. Inskip, P. Croft, L. Campbell and C. Cooper, "Osteoarthritis of the hip and occupational lifting," Am J Epidemiol, vol. 147, no. 6, pp. 523-528, 1998. View Article
[22] P. Croft, D. Coggon, M. Cruddas and C. Cooper, "Osteoarthritis of the hip: an occupational disease in farmers," Bmj, vol. 304, no. 6837, pp. 1269-1272, 1992. View Article
[23] M. A. Davis, W. H. Ettinger, J. M. Neuhaus, S. A. Cho and W. W. Hauck, "The association of knee injury and obesity with unilateral and bilateral osteoarthritis of the knee," Am J Epidemiol, vol. 130, no. 2, pp. 278-288, 1989. View Article
[24] J. J. Anderson and D. T. Felson, "Factors associated with osteoarthritis of the knee in the first National Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work," Am J Epidemiol, vol. 128, pp. 179-189, 1988. View Article
[25] J. Dequeker and J. Aerssens, "Bone mineral density and osteoarthritis," Ann Rheum Dis, vol. 52, no. 4, p. 316, 1993. View Article
[26] D. J. Hart, I. Mootoosamy, D. V. Doyle and T. D. Spector, "The relationship between osteoarthritis and osteoporosis in the general population: the Chingford Study," Ann Rheum Dis, vol. 53, pp. 158-162, 1994. View Article
[27] C. Cooper, P. L. Cook, C. Osmond, L. Fisher and M. I. Cawley, "Osteoarthritis of the hip and osteoporosis of the proximal femur," Ann Rheum Dis, vol. 50, pp. 540-542, 1991. View Article
[28] F. A. Burgener, S. P. Meyers, R. K. Tan and W. Zaunbauer, "Differential diagnosis in magnetic resonance imaging," Radiology and Nuclear Medicine, vol. 33, no. 17, p. 663, 2002. View Article
[29] W. Platzer, "Locomotor System," Color Atlas of Human Anatomy Hradec Králové, vol. 47, no. 2, p. 147, 2004. View Article
[30] T. J. Fairbank, "Knee joint changes after meniscectomy," J Bone Joint Surg Br, vol. 30, no. 4, pp. 664-670, 1948. View Article
[31] J. Martel-Pelletier, "Pathophysiology of osteoarthritis," Osteoarthritis Cartilage, vol. 12, pp. 31-33, 2004. View Article
[32] R. D. Altman, "Classification of disease: osteoarthritis," Semin Arthritis Rheum , vol. 20, pp. 40-47, 1991. View Article
[33] D. J. Magee, "Knee," in Orthopedic Physical Assessment, St. Louis, MO, Saunders Elsevier, 2013, p. 834. View Book
[34] A. Harilainen, P. Myllynen, J. Rauste and E. Silvennoinen, "Diagnosis of acute knee ligament injuries: the value of stress radiography compared with clinical examination, stability, under anesthesia and arthroscopic or operative findings," Ann Chir Gynaecol, vol. 75, pp. 37-43, 1986. View Article
[35] J. W. Katz and R. J. Fingeroth, "The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries," Am J Sports Med, vol. 14, pp. 88-91, 1986. View Article
[36] R. J. Scholten, W. L. Deville, W. Opstelten, D. Bijl, C. G. Van Der Plas and L. M. Bouter, "The accuracy of physical diagnostic tests for assessing meniscal lesions of the knee: a metaanalysis," J Fam Pract, vol. 50, no. 11, pp. 938-945, 2001. View Article
[37] P. J. Evans, G. D. Bell and C. Y. Frank, "Prospective evaluation of the McMurrayTest," Am J Sports Med, vol. 21, no. 4, pp. 604-608, 1993. View Article
[38] A. Harilainen, "Evaluation of knee instability in acute ligamentous injuries," Ann Chir Gynaecol, vol. 76, pp. 269-273, 1987. View Article
[39] I. F. Petersson, T. Boegård, T. Saxne, A. J. Silman and B. Svensson, "Radiographic osteoarthritis of the knee classified by the Ahlbäck and Kellgren & Lawrence systems for the tibiofemoral joint in people aged 35-54 years with chronic knee pain," Ann Rheum Dis, vol. 56, p. 493-496, 1997. View Article
[40] J. H. Kellgren and J. S. Lawrence, "Radiological assessment of osteo-arthrosis," Ann Rheum Dis, vol. 16, p. 494-502, 1957. View Article
[41] D. C. Bauer, D. J. Hunter, S. B. Abramson, M. Attur, M. Corr, D. Felson, D. Heinegard, J. M. Jordan, T. B. Kepler, N. E. Lane, T. Saxne, B. Tyree and V. B. Kraus, "Classification of osteoarthritis biomarkers: a proposed approach," Osteoarthritis Cartilage, vol. 14, p. 723-727, 2006. View Article
[42] H. J. Braun and G. E. Gold, "Diagnosis of osteoarthritis: imaging," Bone, vol. 51, no. 2, pp. 278-288, 2012. View Article
[43] E. Yusuf, M. C. Kortekaas, I. Watt, T. W. Huizinga and M. Kloppenburg, "Do knee abnormalities visualised on MRI explain knee pain in knee osteoarthritis? A systematic review," Ann Rheum Dis, vol. 70, no. 1, pp. 60-67, 2011. View Article
[44] X. Li, S. Martin, C. Pitris, R. Ghanta, D. L. Stamper, M. Harman, J. G. Fujimoto and M. E. Brezinski, "High-resolution optical coherence tomographic imaging of osteoarthritic cartilage during open knee surgery," Arthritis Res Ther, vol. 7, no. 2, p. R318, 2005. View Article
[45] P. Dieppe, J. Cushnaghan, P. Young and J. Kirwan, "Prediction of the progression of joint space narrowing in osteoarthritis of the knee by bone scintigraphy," Ann Rheum Dis, vol. 52, no. 8, pp. 557-563, 1993. View Article
[46] P. R. Bureau, "Today's Research on Aging," Program and Policy Implications Issue, Washington DC, USA, 2015. View Article
[47] M. Fransen, S. McConnell and M. Bell, "Exercise for osteoarthritis of the hip or knee. Cochrane Database Syst Rev 2001; 2:CD004286," Ann Intern Med, vol. 143, p. 427-438, 2005. View Article
[48] R. Christensen, A. Astrup and H. Bliddal, "Weight loss: the treatment of choice for knee osteoarthritis? A randomized trial," Osteoarthritis Cartilage, vol. 13, no. 1, pp. 20-27, 2005. View Article
[49] C. M. Jenkinson, M. Doherty, A. J. Avery, A. Read, M. A. Taylor, T. H. Sach and e. al, "Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial," Bmj, p. 339, 2009. View Article
[50] N. J. Bosomworth, "Exercise and knee osteoarthritis: benefit or hazard?," Can Fam Physician, vol. 55, pp. 871-878, 2009. View Article
[51] A. Jones, P. G. Silva, A. C. Silva, M. Colucci, A. Tuffanin, J. R. Jardim and e. al, "Impact of cane use on pain, function, general health, and energy expenditure during gait in patients with knee osteoarthritis: a randomised control trial," Ann Rheum Dis, vol. 71, p. 172-179, 2012. View Article
[52] R. W. Brouwer, T. M. Van Raaij, J. A. Verhaar, L. N. Coene and S. M. Bierma-Zeinstra, "Brace treatment for osteoarthritis of the knee: a prospective randomized multi-centre trial," Osteoarthritis Cartilage, vol. 14, no. 8, pp. 777-783, 2006. View Article
[53] D. Bhatia, T. Bejarano and M. Novo, "Current interventions in the management of knee osteoarthritis," J Pharm Bioall Sci, vol. 5, pp. 30-38, 2013. View Article
[54] M. Watson, S. T. Brookes, A. Faulkner and J. Kirwan, Non aspirin, non steroidal anti inflammatory drugs for treating osteoarthritis of the knee, The Cochrane Library, 1997. View Book
[55] N. Bellamy, J. Campbell, V. Welch, T. L. Gee, R. Bourne and G. A. Wells, "Intraarticular corticosteroid for treatment of osteoarthritis of the knee," Cochrane Database Syst Rev, vol. 2, p. CD005328, 2005. View Article
[56] G. H. Lo, M. LaValley, T. McAlindon and D. T. Felson, "Intra-articular hyaluronic acid in treatment of knee osteoarthritis: a meta-analysis," Jama, vol. 290, no. 23, pp. 3115-3121, 2003. View Article
[57] J. Richmond, D. Hunter, J. Irrgang, M. H. Jones, B. Levy, R. Marx and e. al, "Treatment of osteoarthritis of the knee (nonarthroplasty)," J Am Acad Orthop Surg, vol. 17, no. 9, pp. 591-600, 2009. View Article
[58] á. J. Geirsson, S. Statkevicius and A. Víkingsson, "Septic arthritis in Iceland 1990-2002: increasing incidence due to iatrogenic infections," Ann Rheum Dis, vol. 67, no. 5, pp. 638-643, 2008. View Article
[59] T. E. Towheed, L. Maxwell, T. P. Anastassiades, B. Shea, J. B. Houpt, V. Welch and e. al, "Glucosamine therapy for treating osteoarthritis," Cochrane Database Syst Rev, vol. 2, no. 2, 2005. View Article
[60] R. J. Petrella and M. Petrella, "A prospective, randomized, double-blind, placebo controlled study to evaluate the efficacy of intraarticular hyaluronic acid for osteoarthritis of the knee," J Rheumatol, vol. 33, no. 5, pp. 951-956, 2006. View Article
[61] T. H. Trojian, A. L. Concoff, S. M. Joy, J. R. Hatzenbuehler, W. J. Saulsberry and C. I. Coleman, "AMSSN scientific statement concerning viscosupplementation injection for knee osteoarthritis: importance for individual patient outcome," Clin J Sport Med, Br J Sports Med, vol. 50, p. 84-92, 2016. View Article
[62] L. M. Wildi, J. P. Raynauld, J. M. Pelletier, A. Beaulieu, L. Bessette, F. Morin and e. al, "Chondroitin sulphate reduces both cartilage volume loss and bone marrow lesions in knee osteoarthritis patients starting as early as six months after initiation of therapy. A randomised double blind placebo controlled pilot study using MRI," Ann Rheum Dis, vol. 70, pp. 982-989, 2011. View Article
[63] W. Zhang, R. W. Moskowitz, G. Nuki, S. Abramson, R. D. Altman, N. Arden and e. al, "OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence based expert consensus guidelines," Osteoarthritis Cartilage, vol. 16, pp. 137-162, 2008. View Article
[64] J. D. Bradley, K. D. Brandt, B. P. Katz, L. A. Kalasinski and S. I. Ryan, "Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee," N Engl J Med, vol. 325, p. 87-91, 1991. View Article
[65] K. D. Brandt, S. A. Mazzuca and K. A. Buckwalter, "Acetaminophen, like conventional NSAIDS, may reduce synovitis in osteoarthritic knees," Rheumatology, vol. 45, p. 1389-1394, 2006. View Article
[66] M. Underwood, D. Ashby, P. Cross, E. Hennessy, L. Letley, J. Martin and e. al, "Advice to use topical or oral ibuprofen for chronic knee pain in older people: randomised controlled trial and patient preference study," BMJ, vol. 336, no. 7636, pp. 138-142, 2008. View Article
[67] M. C. Hochberg, R. D. Altman, K. T. April, M. Benkhalti, G. Guyatt, J. McGowan and e. al, "American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee," Arthritis Care Res, vol. 64, no. 4, pp. 465-474, 2012. View Article
[68] J. Fond, D. Rodin, S. Ahmad and R. P. Nirschl, "Arthroscopic debridement for the treatment of osteoarthritis of the knee: 2-and 5-year results," Arthroscopy: The Journal of Arthroscopic & Related Surgery, vol. 18, no. 8, pp. 829-834, 2002. View Article
[69] S. V. Herrlin, P. O. Wange, G. Lapidus, M. Hållander, S. Werner and L. Weidenhielm, "Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up," Knee Surg Sports Traumatol Arthrosc, vol. 21, no. 2, pp. 358-364, 2013. View Article
[70] A. Kirkley, T. B. Birmingham, R. B. Litchfield, J. R. Giffin, K. R. Willits, C. J. Wong and e. al, "A randomised trial of arthroscopic surgery for osteoarthritis of the knee," N Engl J Med, vol. 359, pp. 1097-1107, 2008. View Article
[71] D. Matsunaga, S. Akizuki, T. Takizawa, I. Yamazaki and J. Kuraishi, "Repair of articular cartilage and clinical outcome after osteotomy with microfracture or abrasion arthroplasty for medial gonarthrosis," The Knee, vol. 14, no. 6, pp. 465-471, 2007. View Article
[72] M. Brittberg, A. Lindahl, A. Nilsson, C. Ohlsson, O. Isaksson and L. Peterson, "Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation," N Engl J Med, vol. 331, p. 889-895, 1984. View Article
[73] A. G. McNickle, M. T. Provencher and B. J. Cole, "Overview of existing cartilage repair technology," Sports Med Arthrosc Rev, vol. 16, no. 4, pp. 196-201, 2008. View Article
[74] L. Hangody, G. K. Ráthonyi, Z. Duska, G. Vásárhelyi, P. Füles and L. Módis, "Autologous osteochondral mosaicplasty," J Bone Joint Surg Am, vol. 86, no. suppl 1, pp. 65-72, 2004. View Article
[75] L. Hangody, G. Vásárhelyi, L. R. Hangody, Z. Sukosd, G. Tibay, L. Bartha and e. al, "Autologous osteochondral grafting-technique and long-term results," Injury, vol. 39, no. Suppl.1, p. 32-39, 2008. View Article
[76] J. P. Jackson and W. Waugh, "Tibial osteotomy for osteoarthritis of the knee," J Bone Joint Surg Br, vol. 43, pp. 746-751, 1961. View Article
[77] T. C. Kienzle III, S. D. Stulberg, M. Peshkin, A. Quaid, J. Lea, A. Goswani and C. H. Wu, "Total knee replacement," Engineering in Medicine and Biology Magazine, IEEE, vol. 14, no. 3, pp. 301-306, 1995. View Article
[78] J. Singh, "Ultrasonic Therapy," in Textbook of electrotherapy, New Delhi, Jaypee Brothers Medical Publishers, 2012, p. 267. View Article
[79] R. Melzack, "Gate control theory: On the evolution of pain concepts," In Pain forum, vol. 5, no. 2, pp. 128-138, 1996. View Article
[80] R. Melzack and P. D. Wall, "Pain mechanisms: a new theory," Survey of Anesthesiology, vol. 11, no. 2, pp. 89-90, 1967. View Article
[81] V. Robertson, A. Ward, J. Low and A. Reed, Forword Lynn Snyder-Mackler. Electrotherapy explained. Principles and practice, Oxford: Butterworth Heinemann, 2006. View Book
[82] P. Dehail, C. Duclos and M. Barat, "Electrical stimulation and muscle strengthening," Ann Readapt Med Phys, vol. 51, no. 6, pp. 441-451, 2008. View Article
[83] B. V. Reed, "Effect of high voltage pulsed electrical stimulation on microvascular permeability to plasma protein. A possible mechanism in minimizing edema," Phys Ther, vol. 68, pp. 491-495, 1988. View Article
[84] J. A. Feedar, L. C. Kloth and G. D. Gentzkow, "Chronic dermal ulcer healing enhanced with monophasic pulsed electrical stimulation," Phys Ther, vol. 71, pp. 639-649, 1991. View Article
[85] F. Tok, K. Aydemir, F. Peker, I. Safaz, M. A. Taşkaynatan and A. Ozgül, "The effects of electrical stimulation combined with continuous passive motion versus isometric exercise on symptoms, functional capacity, quality of life and balance in knee osteoarthritis: randomized clinical trial," Rheumatol Int, vol. 31, no. 2, p. 177-181, 2011. View Article
[86] Y. Escalante, A. García-Hermoso and J. M. Saavedra, "Effects of exercise on functional aerobic capacity in lower limb osteoarthritis: a systematic review," J Sci Med Sport, vol. 14, no. 3, p. 190-198, 2011. View Article
[87] J. B. Thorlund, P. Aagaard and E. M. Roos, "Muscle strength and functional performance in patients at high risk of knee osteoarthritis: a follow-up study," Knee Surg Sports Traumatol Arthrosc, vol. 20, no. 6, p. 1110-1117, 2011. View Article
[88] M. G. Rosemffet, E. E. Schneeberger, G. Citera, M. E. Sgobba, C. Laiz, H. Schmulevich, P. Artçanuturry, S. Gagliardi and J. A. Maldonado Cocco, "Effects of functional electrostimulation on pain, muscular strength, and functional capacity in patients with osteoarthritis of the knee," J Clin Rheumatol, vol. 10, no. 5, p. 246-249, 2004. View Article
[89] J. F. Holla, M. van der Leeden, L. D. Roorda, S. M. Bierma-Zeinstra, J. Damen, J. Dekker and M. P. Steultjens, "Diagnostic accuracy of range of motion measurements in early symptomatic hip and/or knee osteoarthritis," Arthritis Care Res, vol. 64, no. 1, p. 59-65, 2012. View Article
[90] M. L. Cammarata and Y. Y. Dhaher, "Associations between frontal plane joint stiffness and proprioceptive acuity in knee osteoarthritis," Arthritis Care Res, vol. 64, no. 5, p. 735-743, 2012. View Article
[91] A. Elbaz, E. M. Debbi, G. Segal, A. Haim, N. Halperin, G. Agar, A. Mor and R. Debi, "Sex and body mass index correlate with Western Ontario and McMaster Universities Osteoarthritis Index and quality of life scores in knee osteoarthritis," Arch Phys Med Rehabil, vol. 92, no. 10, p. 1618-1623, 2011. View Article
[92] A. C. Gelber, "Osteoarthritis research: current state of the evidence," Curr Opin Rheumatol, vol. 27, p. 273-275, 2015. View Article
[93] J. D. Childs, P. J. Sparto, G. K. Fitzgerald, M. Bizzini and J. J. Irrgang, "Alterations in lower extremity movement and muscle activation patterns in individuals with knee osteoarthritis," Clin Biomech, vol. 19, p. 44-49, 2004. View Article
[94] C. Hubley-Kozey, K. Deluzio and M. Dunbar, "Muscle co-activation patterns during walking in those with severe knee osteoarthritis," Clin Biomech, vol. 23, no. 1, pp. 71-80, 2008. View Article
[95] A. N. Gam and F. Johannsen, "Ultrasound therapy in musculoskeletal disorders: a metaanalysis," Pain, vol. 63, no. 1, pp. 85-91, 1995. View Article
[96] D. A. van der Windt, G. J. van der Heijden, S. G. van den Berg, G. ter Riet and A. F. B. L. M. de Winter, "Ultrasound therapy for musculoskeletal disorders: a systematic review," Pain, vol. 81, no. 3, pp. 257-271, 1999. View Article
[97] J. Falconer, K. W. Hayes and R. W. Chang, "Effect of ultrasound on mobility in osteoarthritis of the knee. A randomized clinical trial," Arthritis Rheum, vol. 5, no. 1, pp. 29-35, 1992. View Article
[98] R. A. Wong, B. Schumann, R. Townsend and C. A. Phelps, "A survey of therapeutic ultrasound use by physical therapists who are orthopaedic certified specialists," Phys Ther, vol. 87, no. 8, pp. 986-994, 2007. View Article
[99] N. Cetin, A. Aytar, A. Atalay and M. N. Akman, "Comparing hot pack, short-wave diathermy, ultrasound, and TENS on isokinetic strength, pain, and functional status of women with osteoarthritic knees: a single-blind, randomized, controlled trial," Am J Phys Med Rehabil, vol. 87, no. 6, pp. 443-451, 2008. View Article
[100] L. ÖzgÖnenel, E. Aytekin and G. Durmuşoǧlu, "A double-blind trial of clinical effects of therapeutic ultrasound in knee osteoarthritis," Ultrasound Med Biol, vol. 35, no. 1, pp. 44-49, 2009. View Article
[101] G. Jamtvedt, K. T. Dahm, A. Christie, R. H. Moe, E. Haavardsholm, I. Holm and K. B. Hagen, "Physical therapy interventions for patients with osteoarthritis of the knee: an overview of systematic reviews," Phys Ther, 2007. View Article
[102] J. Z. Srbely, "Ultrasound in the management of osteoarthritis: Part 1: a review of the current literature," J Can Chiropr Assoc, vol. 52, no. 1, p. 30, 2008. View Article
[103] F. Tascioglu, S. Kuzgun, O. Armagan and G. Ogutler, "Short-term effectiveness of ultrasound therapy in knee osteoarthritis," J Int Med Res, vol. 38, no. 4, pp. 1233-1242, 2010. View Article
[104] A. Loyola-Sánchez, J. Richardson and N. J. MacIntyre, "Efficacy of ultrasound therapy for the management of knee osteoarthritis: a systematic review with meta-analysis," Osteoarthritis Cartilage, vol. 18, no. 9, pp. 1117-1126, 2010. View Article
[105] A. W. Rutjes, E. Nüesch, R. Sterchi and P. Jüni, "Therapeutic ultrasound for osteoarthritis of the knee or hip," Cochrane Database Syst Rev, vol. 1, no. 1, 2010. View Article
[106] M. Muftic and K. Miladinovic, "Therapeutic Ultrasound and Pain in Degenerative Diseases of Musculoskeletal System," Acta Informatica Medica, vol. 21, no. 3, p. 170, 2013. View Article
[107] M. Osiri, V. Welch, L. Brosseau, B. Shea, J. McGowan, P. Tugwell and G. Wells, "Transcutaneous electrical nerve stimulation for knee osteoarthritis," Cochrane Data Base Syst Rev, 2001. View Article
[108] K. A. Sluka and D. Walsh, "Transcutaneous electrical nerve stimulation: basic science mechanisms and clinical effectiveness," The Journal of Pain, vol. 4, no. 3, pp. 109-121, 2003. View Article
[109] G. L. Y. Cheing, A. Y. Y. Tsui, S. K. Lo and C. W. Y. HuiChan, "Optimal stimulation duration of TENS in the management of osteoarthritis knee pain," J Rehabil Med, vol. 35, pp. 62-68, 2003. View Article
[110] P. P. Law, G. L. Cheing and A. Y. Tsui, "Does transcutaneous electrical nerve stimulation improve the physical performance of people with knee osteoarthritis?," J Clin Rheumatol, vol. 10, no. 6, pp. 295-299, 2004. View Article
[111] K. Itoh, S. Hirota, Y. Katsumi, H. Ochi and H. Kitakoji, "A pilot study on using acupuncture and transcutaneous electrical nerve stimulation (TENS) to treat knee osteoarthritis (OA)," Chin Med, vol. 3, no. 2, 2008. View Article
[112] J. M. Bjordal, M. I. Johnson, R. A. Lopes-Martins, B. Bogen, R. Chow and A. E. Ljunggren, "Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials," BMC Musculoskelet Disord, vol. 8, no. 1, p. 1, 2007. View Article
[113] A. W. S. Rutjes, E. Nüesch, R. Sterchi, L. Kalichman, E. Hendriks, M. Osiri, L. Brosseau, S. Reichenbach and P. Jüni, "Transcutaneous electrostimulation for osteoarthritis of the knee," Cochrane Database of Systematic Reviews, no. 4, 2009. View Article
[114] A. Wright, "Exploring the evidence for using TENS to relieve pain," Nursing Times, 2012. View Article
[115] C. G. Vance, D. L. Dailey, B. A. Rakel and K. A. Sluka, "Using TENS for pain control: the state of the evidence," Pain management, vol. 4, no. 3, pp. 197-209, 2014. View Article
[116] D. A. Lake, "Neuromuscular electrical stimulation," Sports medicine, vol. 13, no. 5, pp. 320-336, 1992. View Article
[117] J. P. Porcari, J. Miller, K. Cornwell, C. Foster, M. Gibson, K. McLean and e. al, "Back Issues," J Sports Sci Med, vol. 4, pp. 66-75, 2005.
[118] R. M. Palmieri-Smith, A. C. Thomas, C. Karvonen-Gutierrez and M. Sowers, "A clinical trial of neuromuscular electrical stimulation in improving quadriceps muscle strength and activation among women with mild and moderate osteoarthritis," Phys ther, vol. 90, no. 10, pp. 1441-1452, 2010. View Article
[119] J. Gondin, P. J. Cozzone and D. Bendahan, "Is high-frequency neuromuscular electrical stimulation a suitable tool for muscle performance improvement in both healthy humans and athletes?," Eur J Appl Physiol, vol. 111, no. 10, pp. 2473-2487, 2011. View Article
[120] R. A. Bruce-Brand, R. J. Walls, J. C. Ong, B. S. Emerson, J. M. O'Byrne and N. M. Moyna, "Effects of home-based resistance training and neuromuscular electrical stimulation in knee osteoarthritis: a randomized controlled trial," BMC Musculoskelet Disord, vol. 13, no. 1, p. 1, 2012. View Article
[121] M. de Oliveira Melo, F. A. Aragão and M. A. Vaz, "Neuromuscular electrical stimulation for muscle strengthening in elderly with knee osteoarthritis-a systematic review," Complement Ther Clin Pract, vol. 19, no. 1, pp. 27-31, 2013. View Article
[122] M. A. Vaz, B. M. Baroni, J. M. Geremia, F. J. Lanferdini, A. Mayer, A. Arampatzis and W. Herzog, "Neuromuscular electrical stimulation (NMES) reduces structural and functional losses of quadriceps muscle and improves health status in patients with knee osteoarthritis," J Orthop Res, vol. 31, no. 4, pp. 511-516, 2013. View Article
[123] A. Mizusaki Imoto, S. Peccin, K. N. Gomes da Silva, L. E. de Paiva Teixeira, M. I. Abrahão and V. Fernandes Moça Trevisani, "Effects of neuromuscular electrical stimulation combined with exercises versus an exercise program on the pain and the function in patients with knee osteoarthritis: a randomized controlled trial," in BioMed research international, 2013. View Article
[124] T. M. Zizic, K. C. Hoffman, P. A. Holt, D. S. Hungerford, J. R. O Dell, M. A. Jacobs and e. al, "The treatment of OA of the knee with pulsed electrical stimulation," J Rheumatol, vol. 22, pp. 1757-1761, 1995. View Article
[125] J. Farr, M. A. Mont, D. Garland, J. R. Caldwell and T. M. Zizic, "Pulsed electrical stimulation in patients with osteoarthritis of the knee: follow up in 288 patients who had failed non-operative therapy," Surg Technol Int, vol. 15, pp. 227-233, 2005. View Article
[126] D. Garland, P. Holt, J. T. Harrington, J. Caldwell, T. M. Zizic and J. Cholewczynski, "A 3- month randomised double blind placebo controlled study to evaluate the safety and efficacy of highly optimised capacitively coupled, pulsed electrical stimulator in patients with osteoarthritis of the knee," Osteoarthritis Cartilage, vol. 15, pp. 630-637, 2007. View Article
[127] R. E. Fary, N. K. Briffa and T. G. Briffa, "Effectiveness of pulsed electrical stimulation in the management of osteoarthritis of the knee: Three case reports," Physiother Theory Pract, vol. 25, no. 1, p. 21-29, 2009. View Article
[128] R. E. Fary, G. J. Carroll, T. G. Briffa and N. K. Briffa, "The effectiveness of pulsed electrical stimulation in the management of osteoarthritis of the knee: Results of a double-blind, randomized, placebo-controlled, repeated-measures trial," Arthritis Rheum, vol. 63, no. 5, p. 1333-1342, 2011. View Article
[129] A. Negm, A. Lorbergs and N. J. MacIntyre, "Efficacy of low frequency pulsed subsensory threshold electrical stimulation vs placebo on pain and physical function in people with knee osteoarthritis: systematic review with meta-analysis," Osteoarthritis Cartilage, vol. 21, pp. 1281-1289, 2013. View Article
[130] T. A. o. EMG, A Practical Introduction to Kinesiological Electromyography, Noraxon Inc., 2006.
[131] S. M. McGill, "A myoelectrically based dynamic three-dimensional model to predict loads on lumbar spine tissues during lateral bending," Journal of biomechanics, vol. 25, no. 4, pp. 395-414, 1992. View Article
[132] D. G. Lloyd and T. F. Besier, "An EMG-driven musculoskeletal model to estimate muscle forces and knee joint moments in vivo," Journal of biomechanics, vol. 36, no. 6, pp. 765-776, 2003. View Article
[133] D. Bhatia, R. P. Tewari, S. Ayub, K. K. Shukla and M. A. Ansari, "Study the role of muscle under different loading condition," Advances in Applied Science Research, vol. 1, no. 3, pp. 118-128, 2010.
[134] L. G. Hallen and O. Lindahl, "Muscle Function in Knee Extension an EMG Study," Acta orthopaedica Scandinavica, vol. 38, no. 1-4, pp. 434-444, 1967. View Article
[135] R. Drake, A. W. Vogl and A. W. Mitchell, "Gray's anatomy for students," Elsevier Health Sciences, 2014. View Article
[136] L. Shamir, S. M. Ling, W. W. Scott, A. Bos, N. Orlov, T. J. Macura, D. M. Eckley, L. Ferrucci and I. G. Goldberg, "Knee X-ray image analysis method for automated detection of Osteoarthritis," IEEE Transactions on Biomedical Engineering, vol. 56, no. 2, pp. 407-415, 2009. View Article
[137] O. O. Yılmaz, O. Senocak, E. Sahin, M. Baydar, S. Gulbahar, C. Bircan and S. Alper, "Efficacy of EMG-biofeedback in knee osteoarthritis," Rheumatology international, vol. 30, no. 7, pp. 887-892, 2010. View Article
[138] T. Hortobágyi, L. Westerkamp, S. Beam, J. Moody, J. Garry, D. Holbert and P. DeVita, "Altered hamstring-quadriceps muscle balance in patients with knee osteoarthritis," Clinical Biomechanics, vol. 20, no. 1, pp. 97-104, 2005. View Article
[139] C. L. Hubley-Kozey, K. J. Deluzio, S. C. Landry, J. S. McNutt and W. D. Stanish, "Neuromuscular alterations during walking in persons with moderate knee osteoarthritis," Journal of Electromyography and Kinesiology, vol. 16, no. 4, pp. 365-378, 2006. View Article
[140] J. A. Zeni, K. Rudolph and J. S. Higginson, "Alterations in quadriceps and hamstrings coordination in persons with medial compartment knee osteoarthritis," Journal of Electromyography and Kinesiology, vol. 20, no. 1, pp. 148-154, 2010. View Article
[141] D. T. Barry, K. E. Gordon and G. G. Hinton, "Acoustic and surface EMG diagnosis of pediatric muscle disease," Muscle & nerve, vol. 13, no. 4, pp. 286-290, 1990. View Article
[142] A. Berardelli, J. P. Dick, J. C. Rothwell, B. L. Day and C. D. Marsden, "Scaling of the size of the first agonist EMG burst during rapid wrist movements in patients with Parkinson's disease," Journal of Neurology, Neurosurgery & Psychiatry, vol. 49, no. 11, pp. 1273-1279, 1986. View Article
[143] G. De Michele, S. Sello, M. C. Carboncini, B. Rossi and S. K. Strambi, "Cross-correlation time-frequency analysis for multiple EMG signals in Parkinson's disease: a wavelet approach," Medical engineering & physics, vol. 25, no. 5, pp. 361-369, 2003. View Article
[144] J. P. Callaghan, J. L. Gunning and S. M. McGill, "The relationship between lumbar spine load and muscle activity during extensor exercises," Physical Therapy, vol. 78, no. 1, pp. 8-18, 1998. View Article
[145] M. A. Mont, D. S. Hungerford, J. R. Caldwell, K. C. Hoffman, P. S. Ragland, Y. D. He, L. C. Jones and T. M. Zizic, "Pulsed electrical stimulation to defer TKA in patients with knee osteoarthritis," Orthopedics, vol. 29, no. 10, pp. 887-892, 2006. View Article
[146] A. C. Gelber, "Osteoarthritis research: current state of the evidence," Curr Opin Rheumatol, vol. 27, p. 273-275, 2015. View Article

